Data Collection and Input
I. Traditional EHRs:
Manual Data Entry:
Providers must enter data manually, which can be time-consuming and prone to human error. Information is often in predefined formats like checkboxes or drop-down lists, which can limit the detail of patient records Traditional EHRs VS AI-powered EHR systems.
Unstructured Data Challenges:
Notes, observations, and treatment plans often remain in unstructured text formats, making them difficult to analyze without additional processing.
Data Redundancy:
Repetitive data entry, as information needs to be repeatedly input for similar types of records, often due to lack of integration across departments or facilities.
II. AI-Powered EHRs:
Automated Data Entry:
AI tools, including NLP and voice recognition, capture data from spoken interactions and written notes, converting unstructured text into structured data for analysis.
Data Validation and Quality Improvement:
AI can flag inconsistencies or missing information, which helps maintain higher data accuracy and completeness Traditional EHRs VS AI-powered EHR systems.
Advanced Data Collection (IoT):
Integration with IoT devices, wearables, and home monitoring systems provides real-time data, enabling continuous patient monitoring and better capturing of health metrics.
Data Analysis and Insights
I. Traditional EHRs:
Basic Reporting:
Limited to historical data with minimal prediction capabilities. Reports typically summarize information but lack predictive insights or customized reporting options.
Static Metrics:
Data analysis is often limited to standard health indicators without the capability to identify complex patterns or trends across multiple variables.
II. AI-Powered EHRs:
Predictive Analytics:
Uses machine learning algorithms to predict patient outcomes, disease progression, and potential complications based on historical and current data.
Trend Analysis and Risk Stratification:
AI can identify high-risk patients or populations and suggest preventive interventions by spotting emerging patterns in data Vexed Solutions.
Personalized Health Insights:
AI tailors insights and recommendations to individual patients, taking into account factors like genetic data, lifestyle habits, and environmental influences.
Clinical Decision Support (CDS)
I. Traditional EHRs:
Rule-Based Alerts:
Provides simple rule-based alerts and reminders (e.g., for allergies, drug interactions, or upcoming screenings). While helpful, these are often generic and can lead to alert fatigue.
Limited Guidance:
Basic decision support is limited to preset guidelines and lacks real-time, adaptive support in complex cases.
II. AI-Powered EHRs:
Contextualized Recommendations:
AI can prioritize alerts based on patient context, reducing alert fatigue. It provides recommendations tailored to each patient, making CDS more relevant and actionable.
Real-Time Diagnostics and Imaging Support:
AI algorithms assist in analyzing imaging data (e.g., CT scans, MRIs), lab results, and genetic tests, aiding in quicker and more accurate diagnostics.
Adaptive Learning:
AI learns from new data over time, allowing the CDS to improve and adjust guidelines based on emerging research, practice trends, and specific patient needs.
Patient Engagement
I. Traditional EHRs:
Portal Access:
Patients can access records, message providers, and view test results. However, interactions are often limited to viewing and scheduling, without personalized insights.
Static Information:
Patients receive information but have limited tools for actively managing health or understanding their condition beyond the basics.
II. AI-Powered EHRs:
Personalized Health Recommendations:
AI can deliver tailored advice on lifestyle changes, medication adherence, and preventive measures based on each patient’s history and real-time health data.
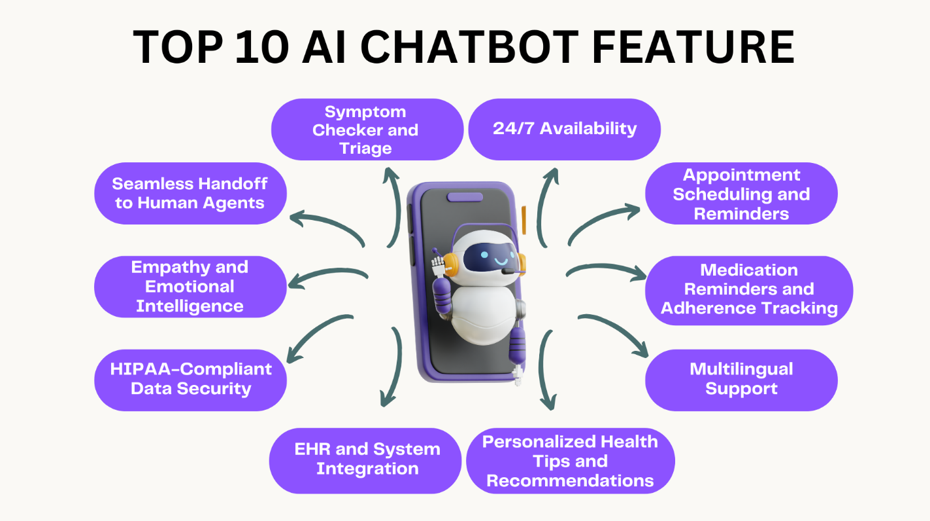
Virtual Health Assistants:
AI-powered chatbots and virtual assistants can answer common questions, provide medication reminders, and even guide patients through post-op care steps.
Continuous Monitoring:
Integration with wearable devices enables remote monitoring and immediate feedback, helping patients stay engaged and take preventive actions when anomalies are detected.
Interoperability and Integration
I. Traditional EHRs:
Fragmented Systems:
Many EHR systems are unable to effectively communicate across different healthcare networks, leading to data silos and duplicative testing or treatments.
Standardization Issues:
Different EHR systems may use different coding systems, data formats, and protocols, making data exchange and integration challenging.
II. AI-Powered EHRs:
Cross-System Compatibility:
AI algorithms can adapt data from various sources, making it easier to integrate data from disparate systems, even those outside traditional healthcare environments.
Data Mapping and Translation:
AI can translate and map data across platforms (such as from ICD codes to SNOMED) for smoother data exchange and compatibility.
Enhanced Population Health Management:
AI-powered interoperability improves coordination of care across different providers, enabling a comprehensive view of patient health and more accurate public health insights.
Operational Efficiency and Workflow Optimization
I. Traditional EHRs:
Manual Workflows:
Routine administrative tasks like patient scheduling, billing, and record management are often manually performed, leading to inefficiency and increased costs.
High Documentation Time:
Extensive documentation requirements can contribute to clinician burnout, with significant time spent on data entry rather than patient care.
II. AI-Powered EHRs:
Automated Task Management:
AI can schedule appointments, streamline billing processes, and reduce administrative workload by handling routine tasks automatically.
Smart Documentation Assistance:
AI-enabled tools help clinicians by automatically summarizing and structuring clinical notes, saving time and reducing error.
Efficient Resource Allocation:
AI can analyze patient flow and suggest adjustments to optimize resources (like beds, staff, and medical equipment), improving overall efficiency and reducing wait times Traditional EHRs VS AI-powered EHR systems.
Security and Privacy
I. Traditional EHRs:
Basic Security Protocols:
Standard security protocols include passwords, multi-factor authentication, and encryption, but these systems can be vulnerable to data breaches.
Limited Threat Detection:
Traditional systems often lack advanced monitoring for detecting sophisticated threats, increasing the risk of unauthorized access or data theft.
II. AI-Powered EHRs:
Advanced Threat Detection:
AI systems use machine learning to identify unusual patterns in data access or user behavior, flagging potential threats and preventing breaches.
Data Privacy Preservation:
AI algorithms can help anonymize and securely handle data, even across systems, while maintaining compliance with regulations like HIPAA or GDPR.
Proactive Security Measures:
AI can anticipate and patch vulnerabilities, preventing breaches before they happen and ensuring robust protection for sensitive patient data.
Conclusion
Traditional EHRs are simpler, reliable for basic record-keeping, and cost-effective for many healthcare settings but lack advanced capabilities like predictive analytics and personalized decision support.
AI-Powered EHRs offer significant advantages in terms of data accuracy, patient engagement, and proactive care management. However, they come with challenges related to cost, data security, and complexity, requiring a careful implementation approach and ongoing monitoring to ensure ethical and accurate usage.